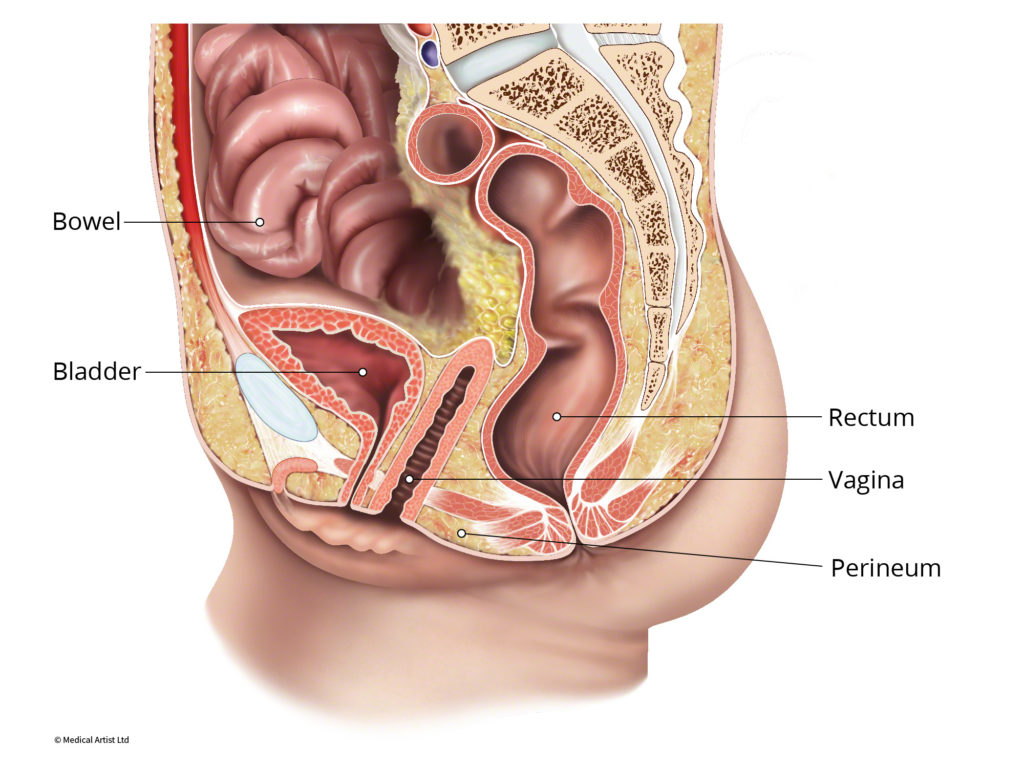
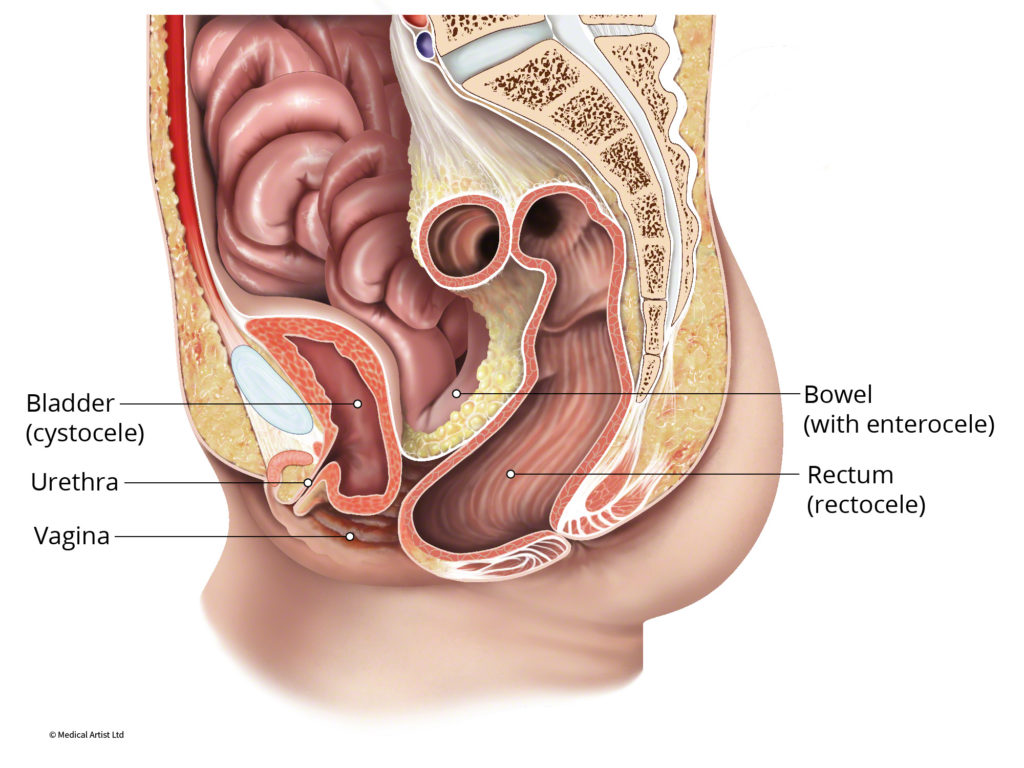
Pelvic organ prolapse refers to a pelvic organ (the uterus, bladder, small intestine or rectum) dropping out of its usual anatomic position into the vaginal canal. An Enterocele or Vaginal Vault Prolapse refers to the fatty tissue around the intestines descending into the lower pelvic cavity forming a bulge into the vagina. In severe cases, parts of the small intestine descend into the vagina. Vaginal vault prolapse occurs in women who have undergone a hysterectomy and develop a loss of support at the top of the vagina. This does not occur in all women who have undergone a hysterectomy but can develop in women with additional risk factors to develop pelvic organ prolapse.
Enterocele
An enterocele can also be present in patients who have a uterus and develop prolapse but is not as common. When this is the case, fatty tissue around the intestines descends into the pelvic cavity and forms a bulge between the cervix and the vagina.
Symptoms can include:
- A feeling of pelvic fullness, pressure or pain. The discomfort is often worse at the end of the day or with heavy lifting.
- Low back pain that improves when lying down
- A soft bulge of tissue in the vagina that increases in size with standing or with activity, and decreases in size when lying down.
- Vaginal discomfort and painful intercourse (dyspareunia)
Book An Appointment
I am very satisfied with the treatment I received: da Vinci Sacrocolpoperineopexy to correct my conditions of cystocele (pelvic organ prolapse) and enterocele (vaginal vault prolapse). I had been treated for interstatial cystitus by another urologist since 2007 after having frequent urinary tract infections. In the fall of 2015 I was diagnosed by this urologist with the vaginal vault prolapse. At that time I searched out Dr. Shoshoua. The staff was very helpful both over the phone and upon my initial visit. I had the robiotic surgery in February and in the same surgery another doctor repaired my left inguinal hernia. It is now six weeks since surgery and my conditions have improved. Very minimal bladder leakage and the bulge is gone.
-Evelyn W.
The main factors that contribute to the development of an enterocele are:
- Prior hysterectomy. If the uterus was removed in the past and prolapse develops, an enterocele will be present.
- Hereditary factors. Some women are genetically predisposed to having weaker connective tissues and may be more likely to experience enterocele.
- Childbirth. Vaginal birth can stretch and weaken the supporting structures of the pelvic floor.
- Age. As supporting structures of the pelvic floor age, they weaken.
An enterocele is diagnosed by pelvic exam. Often times, other defects of the pelvic floor are present, such as cystocele and rectocele.
Early stage enterocele may not require treatment. Non-surgical options may help symptoms, but will not fix the prolapse (bulge). Symptoms of prolapse may improve with pelvic floor physical therapy. A pessary is typically used in women who are not candidates for surgery due to age or poor health. A pessary can limit intercourse and therefore may not be a good option for sexually active women who are able to tolerate surgery.
Surgery for enterocele is elective and is done to relieve symptoms. Surgery may be robotic or vaginal. There are several different surgical techniques to repair an enterocele based on the size of the enterocele and the presence of other prolapsed organs.
Got questions? Need an appointment? We’re here to help!